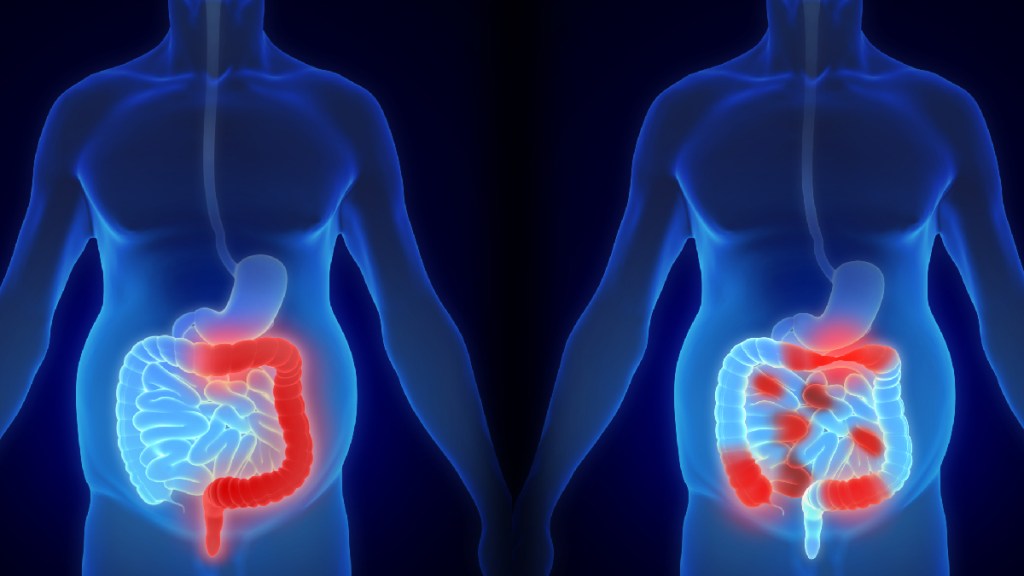
According to an estimate, about one million people in the US suffer from ulcerative colitis. Stats from different parts of the world suggest that IBD is three times more prevalent compared to Crohn’s disease. A significantly large group of patients with UC remain underserved because they show little to no symptoms. When IBD affects the last 15 centimeters of the colon, it is known as ulcerative proctitis. About 25% to 55% of IBD patients are diagnosed with ulcerative proctitis. Patients with ulcerative colitis that is not advanced enough to require biological medications are often not included in the clinical trials of IBD treatment drugs.
Experts take a special interest in studying the impact of IBD on the gut microbiome. The microbiome includes fungi, viruses, bacteria, and other biomes that live in the body. Experts are currently striving to understand how changing the makeup of gut bacteria can affect the development of IBD. Since there is not much evidence available in this regard, experts are yet to know if the microbiome can help treat IBD.
Some evidence, however, suggests that antibiotics may be helpful in some cases to manage some symptoms or complications of IBD. This treatment approach is not without complications, though. Antibiotic treatment is usually a short-term measure because a majority of people have a lower tolerance to antibiotics. That makes the occurrence of adverse effects a more likely outcome. Moreover, the lack of understanding of how an antibiotic treatment can be effective at a particular stage in some cases but not the others is also a point of concern for medical experts. Any antibiotic treatment aims at killing the bad bacteria in the gut, but the good bacteria are also killed in the process. As a result, this treatment can cause worsened symptoms in some cases.
During the IBD Innovate, a conference held to bring together researchers and startups to introduce new treatment options for patients with IBD, Dr. Gil Melmed, Co-Director of the Inflammatory Bowel Disease Center at Cedars-Sinai Medical Center, said that a new device may help treat less severe cases of IBD.
UV light therapy for ulcerative colitis treatment
In recent years, experts haven’t been paying attention to discovering treatment options for mild ulcerative colitis cases. Traditional treatment methods may prove to be more harmful in this regard due to their several drawbacks. That is why there are always several opportunities available to find treatment options to help patients with mild cases.
One of those opportunities is the use of ultraviolet light. Mucosal disease is generally within the reach of UV waves. The light then modulates the affected part of the colon by changing its inflammatory pathways.
UV light can be seen by the naked eye. This light is largely antimicrobial. In case you wonder, UV light is already being used to treat several conditions. For instance, phototherapy is used in the treatment of skin inflammatory disorders.
It raises the question of whether or not UV light can be used for the treatment of IBD. Since it has helped modulate inflammatory pathways, experts hope that they can use different wavelengths of UV light to make it applicable in IBD cases.